The levodopa + carbidopa and vitamin D interaction is apparently additive however the evidence is limited. Given Parkinson’s Disease is considered the number 1 neurological nasty, this is quite surprising.
Parkinsons Disease (PD) is primarily a dopamine deficiency that causes loss in the substantia nigra component of the brain.
As PD is currently considered incurable, management remains symptom-based with levodopa being the primary intervention. Dyskinesia typically manifests within 10 years of commencement of levodopa. The Levodopa-Induced Dyskinesia (LID) is being attributed to dopamine (DA) toxicity, oxidative stress and induction of inflammatory responses. The drugs amantadine and clozapine confer benefit for LID albeit only for a limited duration.
Levodopa + vitamin D positive responses are associated with -
- dopamine metabolism and transport - significant increases in expression of tyrosine hydroxylase, dopamine decarboxylase, dopamine transporter and decreases catechol-o-methyl transferase (COMT) and monoamine oxidase (MAO-B) expression;
- oxidative stress, microglial, inflammation and apoptotic signalling - positive alterations to a range of relevant markers.
The alterations to dopamine metabolism and transport were contradicted 2 years later by the same research group. These studies were related but not similar.
LAT1 (large neutral amino acid transporter1) is one of the levodopa transporters and Vitamin D status may alter its availability. LAT1 functions include mediation of the pH-independent and sodium-independent exchanging transport of the large neutral amino acids (including dopamine), thyroid hormones, and pharmaceutical drugs (including levodopa) across the plasma membrane.
Research in pre-eclampsia has found that -
- reduced placental VDR (Vitamin D Receptor) expression is associated with decreased expression of LAT1;
- vitamin D stimulates LAT1 expression and prevents hypoxia‑induced decrease of LAT1 expression;
- vitamin D upregulates mTOR (Mammalian Target of Rapamycin) signalling via VDR;
- suppression of mTOR pathway downregulates LAT1 expression.
Clinical Considerations
There is a paucity of evidence regarding potential levodopa + carbidopa and vitamin D interactions.
Clarification of vitamin D’s proposed mechanisms of action with levodopa and/or carbidopa would be useful.
Also useful to know is whether the findings with regard to pre-eclampsia, LAT1 and vitamin D translate to neurological function.
Clinical Questions
What actions will you initiate as you a review a person whose prescribed medications include levodopa + carbidopa, will you –
- recommend regular monitoring of vitamin D levels?
- consider recommending a vitamin D intervention?
- recommend the Medications Advisory Committee develop guidelines for vitamin D administration when levodopa + carbidopa is prescribed?
Conclusions
The levodopa + carbidopa and vitamin D interaction still requires further clarification. Seemingly vitamin D may enhance levodopa + carbidopa’s therapeutic effects and reduce it’s negative impacts.
Medical History with Nutritional Aspect
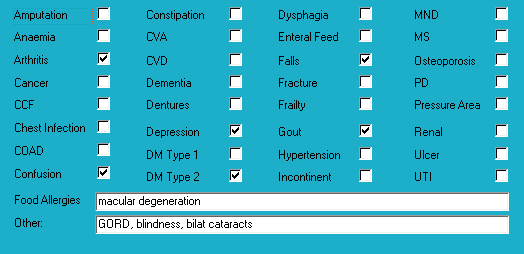
Biochemistry with Nutritional Aspect
No recent relevant results available.
Medications That May Adversely Affect Nutritional Status
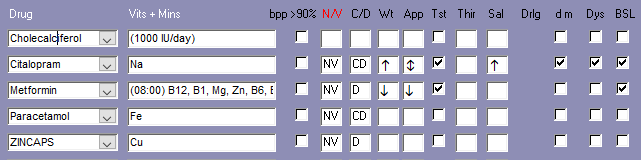
Transporter-mediated interactions and nutrients
Comments – medication and nutrition impacts only
Data summary
Biochemistry
No recent relevant available biochemistry. Advisable to check plasma proteins (albumin, total proteins) as markers of nutritional status.
Glycaemia
BSLs (3 months)
- before breakfast - 6.3-8.1; recommended range 4-6;
- tested weekly;
- reportable limits: < 4 and > 20;
- HbA1c indicates very good overall glycaemic control.
Diabetes drugs
- metformin has a duration of 12 hours.
Diabetes drugs coverage
- before breakfast BSLs - no coverage from previous morning’s metformin;
- before evening meal BSLs - covered by current morning's metformin.
Currently prescribed 3 medications that alter glycaemia.
Pharmaconutrition
Currently prescribed 4 medications that include nausea, vomiting and diarrhoea as side effects.
Currently prescribed 3 medications that include hyperglycaemia as a side effect.
Regular monitoring sodium levels recommended whilst citalopram prescribed.
Currently prescribed vitamin D (1 tab/day). Advisable to check vitamin D levels and if still low then review current vitamin D management strategy.
Coffee inhibits vitamin D uptake by osteoblasts (bone builders) by inhibiting their vitamin D receptors, and consequently decreases calcium and zinc absorption.
Metformin decreases B12 absorption - there is now a recommendation that B12 levels be checked on a regular basis ie at least annually.
Dietary levels of caffeine intake in conjunction with paracetamol inhibit antinocieception.
Paracetamol is a CYP1A2 substrate (can be carried by the transporter). CYP1A2 substrates include caffeine, retinol, melatonin, phosphatidylcholine, inhibitors include grapefruit juice and inducers include coffee; drug’s metabolism inhibited by caffeine therefore drug will remain active in the body for longer.
Concurrent ingestion of paracetamol and iron resulted in increased rate of iron absorption and decreased extent of drug absorption; the authors advise drug and iron to be administered at different times from each other.
Zinc caps have been prescribed for 8 months, and sozole intervention has been ceased therefore advisable to check zinc levels and if well within acceptable range then review necessity for its continued prescription. Zinc and copper share the same absorption mechanism and sustained zinc supplementation may cause a copper deficiency.
Several of the identified membrane transporters inhibit the absorption and/or organ and cellular uptake of thiamine, choline, carnitine, pyridoxine, pantothenate, biotin, folate and vitamin D. Consequently, blood test results may be unreliable due to drug prevention of their entry into or exit from relevant organs and cells. Advisable for blood tests to be conducted several hours after administration of relevant prescribed medicines.
Bowel management
Regular intervention prescribed – No.
PRN interventions prescribed – No.
Nurse Initiated interventions administered – No.
Staff comments
Staff advise Mrs ACV eats well and does not have significant food restrictions.
Observations
Mrs ACV is a small lady with a large abdo and who was lying on her bed when I went to speak to her. She told me she eats well, sleeps well, does not feel upset in the tummy, and sometimes goes outside if the sun is shining.
Mrs ACV has remained remarkably weight stable about 58 kg for the last 3.5 years.
Pharmaconutrition comments
Metformin is administered in the mornings therefore advisable to check afternoon/before-evening meal glycaemia for 3 days and clarify status. Staff advise Mrs ACV does occasionally graze in the afternoons. Mrs ACV's diabetes management includes 1 drug administered before breakfast and which has a duration of about 12 hours. If the 3 days of afternoon glycaemia monitoring indicate hyperglycaemia then it could mean -
1. current medication management strategy is undermedicating glycaemic control and therefore requires review;
2. current medication management strategy is overmedicating glycaemic control and causing the liver to release stored glucose as a hypoglycaemia management strategy and therefore current glycaemia management strategy requires review;
3. current medication management strategy is overmedicating glycaemic control and Mrs ACV is grazing to offset the hypoglycaemic effect and therefore current glycaemia management strategy requires review;
4. current medication management strategy is overmedicating glycaemic control and causing both the liver to release stored glucose and Mrs ACV to graze and therefore current glycaemia management strategy requires review.
Mrs ACV’s diagnoses include arthritis which is typically associated with chronic pain - nutritional factors that may be useful to consider in pain management include -
- vitamin D - current intervention may not be adequate to attain adequate range. Evidence indicates increasingly brittle pain control with decreasing/low vitamin D levels. Advisable to check vitamin D levels and if still low then review current vitamin D management strategy;
- low B12 exacerbates elevated TNF- α which is an inflammatory response marker; elevation of the inflammatory response can include a pain response and currently prescribed metformin therefore advisable to monitor B12 status;
- magnesium – proposed mechanism magnesium blocks the NMDA receptor channels in the spinal cord and thus limits the influx of calcium ie reduces the risk of excitotoxicity and consequent exacerbation of pain. Currently prescribed metformin which decreases magnesium availability. Advisable to monitor magnesium status on a regular basis ie at least annually.
Mrs ACV’s diagnoses include falls - nutritional factors that may be useful to ensure within acceptable ranges include –
-vitamin D – increasing vitamin D intake increases muscle strength and decreases falls; currently prescribed metformin which decreases vitamin D availability therefore advisable to clarify vitamin D status and monitor on a regular basis;
- B12 - is important in the righting reflex when a person stumbles; prescribed metformin therefore advisable to check status;
- Hb – currently prescribed iron therefore advisable to check status;
- magnesium - magnesium is important in vitamin D activation, de novo carnitine production, and muscle function, amongst other functions. Currently prescribed metformin which significantly decreases magnesium availability. Magnesium is an intracellular ion therefore serum levels are unlikely to detect early depletion of status Advisable to clarify magnesium status.
Mitochondrial dysfunction is now being linked to a number of disorders including heart failure, cardiovascular diseases, diabetes, neurodegenerative diseases (MS, Huntingtons, Parkinsons, MND, Alzheimers, glaucoma), ageing, mitochondrial diseases, retinis pigmentosa, CVA, epilepsy, cardiomyopathy, autism, muscular dystrophy, atypical learning disabilities, fibromyalgia, Chronic Fatigue Syndrome, Developmental Delay, Cerebral Palsy, bipolar disorder, major depression disorder, schizophrenia, pulmonary fibrosis, obesity and likely others. Several of Mrs ACV’s diagnoses fall within this umbrella. Whilst the nutritional contribution to neurodegenerative disorders and mitochondrial dysfunction is still in the early stages of research, it is likely nutritional interventions won’t cause harm and will probably confer benefit. Currently prescribed metformin. Nutrients that support dysfunctional mitochondria include -
- magnesium citrate – important in the electron transport chain (etc) and oxidative phosphorylation. Advisable to monitor status on a regular basis ie at least annually;
- if the negative pharmaceutical impacts on transporters is also considered then monitoring of the following is also recommended - thiamine, choline, carnitine, pyridoxine, pantothenate, biotin, folate and vitamin D.
What else would you include?

Yvonne Coleman is an accomplished dietitian with 30+ years of experience in aged care. Her mission is to make information concerning the interactions between medication and nutrition public and easy to access, having created the most comprehensive resource on the matter.
Her areas of competency include food science & nutrition, dietetics and health education. You can find out more about her work on LinkedIn, AusMed, the Enlightened Pharmacist podcast, and The FX Medicine Podcast.


