Levodopa + carbidopa and vitamin C encompass a range of interactions that include both direct and indirect mechanisms of action.
Parkinson’s disease (PD) is a common, progressive neurological nasty for which there is no cure – only management of symptoms. PD’s symptoms typically include tremors, rigidity, slow movement, poor balance, difficulty walking, and facial masking. PD is caused by dopamine deficiency in the brain, predominantly in the substantia nigra and the locus coeruleus. Dopamine’s function is to stimulate the motor neurons that control muscle movement, consequently low levels result in loss of co-ordination.
Proposed mechanisms of action for levodopa + carbidopa and vitamin C include –
1. Direct interactions
Vitamin C –
– directly improves levodopa absorption by preventing magnesium oxide-induced carbidopa breakdown. Maintenance of carbidopa levels means less vitamin B6 being available to decrease levodopa absorption; (Refer MedNut Mail Levodopa + carbidopa, magnesium and vitamin C)
– improves levodopa availability in those with a poor baseline levodopa response;
– decreases the occurrence of levodopa side effects;
– improves drug absorption across the intestinal wall;
– improves reliability in drug delivery as a stabilizer in levodopa + carbidopa solutions.
2. Indirect interactions
There are at least 2 key indirect interactions –
A Oxidative stress
Oxidative stress is the cause of a variety of physiological and pathological conditions. Oxidative stress is the change in the balance between reactive oxygen species (ROS) generation and antioxidant buffering capacity. If ROS is more than the antioxidants capacities then there is direct cellular damage and/or death. Elevated ROS is also likely to cause changes in molecular signalling pathways.
Levodopa + carbidopa side effects include oxidative stress and hyperglycaemia (excessive glucose availability).
Hyperglycaemia can cause increased production of ROS in the mitochondria.
Vitamin C’s significant antioxidant capacity is well known as it has been extensively researched and documented.
Relatively recently investigated were the effects of oxygen pressure in the brain at physiological levels (2% oxygen) on levodopa effects. One of the findings was that levodopa was a ROS scavenger (dampened down the harm). Previous evidence was typically based on normoxic oxygenation (5%).
B GLUT1
The Glucose transporter 1 (GLUT1) is important in –
– the physiological regulation of glucose uptake. Hyperglycaemia activates protein kinase C (PKC) which then phosphorylates GLUT1 to enable rapid glucose uptake;
– dehydroascorbic acid (DHA) transport. Ascorbic acid is transported into neurons by SVCT2 (Sodium Vitamin C Transporter 2), oxidised to DHA and excreted by GLUT3. DHA is then transported into astrocytes by GLUT1, reduced to ascorbic acid, excreted by an unknown transporter, and is available for neuronal uptake again. This neuron-astrocyte link emulates a closed system ie limited nett loss.
GLUT1’s inhibition of DHA transport into astrocytes and subsequent conversion to ascorbic acid means there is a constant loss of ascorbic acid from the closed loop. This loss from the loop creates an increased demand for vitamin C from external sources such as diet.
GLUT1’s inhibition probably means inadequate antioxidant coverage for astrocytes and so they are also at risk of damage and/or death. Each astrocyte services thousands of neurons and thus negative impacts on astrocytes and their functions have profound neurological effects.
Damaged cells cause pain which is a further trigger for ROS and oxidative stress production …
Clinical Considerations
The evidence regarding potential levodopa + carbidopa and vitamin C interactions is quite limited.
The recent finding of significant differences in levodopa’s cellular effects between physiological and normoxic oxygenation has significant implications. If physiological oxygenation is important in levodopa function, then is it also important in the functions of many other drugs? This preliminary evidence does require follow up confirmation.
Recommended daily intakes for most nutrients including vitamin C, based on being healthy (no diagnoses), were established several decades ago. Could a typical daily diet meet the increased vitamin C requirements due to the demands of Parkinson’s Disease and levodopa? What is the increased vitamin C requirement due to levodopa demand?
Clinical Questions
What actions will you initiate as you a review a person whose prescribed medications include levodopa + carbidopa, will you –
- consider recommending a regular ongoing vitamin C intervention?
- recommend the Medications Advisory Committee develop guidelines for vitamin C administration when levodopa + carbidopa is prescribed?
Conclusions
The levodopa + carbidopa and vitamin C interactions impact directly and indirectly including hyperglycaemia, altered absorption and GLUT1 inhibition.
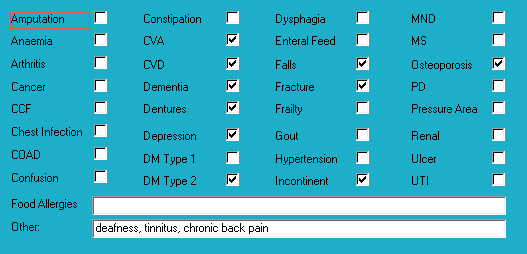
Medical History with Nutritional Aspect
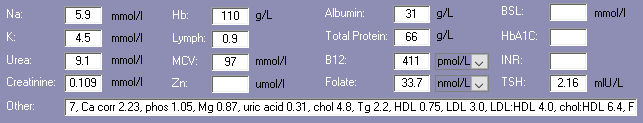
Biochemistry with Nutritional Aspect
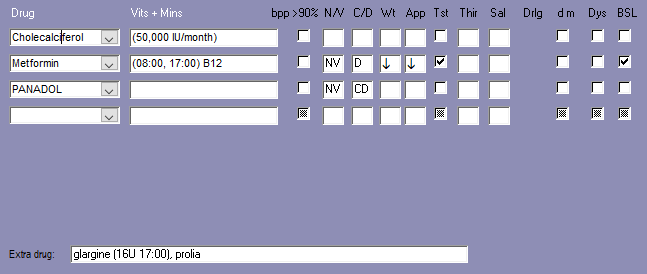
Medications That May Adversely Affect Nutritional Status
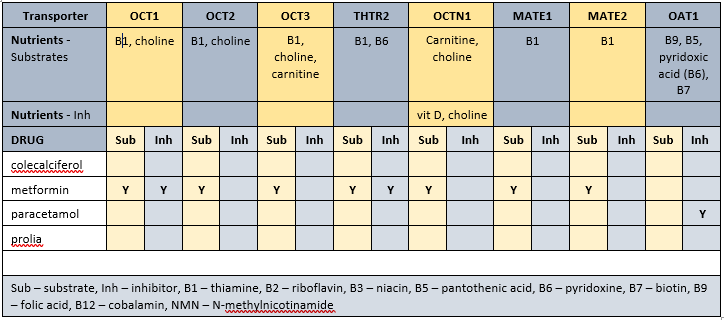
Transporter-mediated interactions and nutrients
Comments – medication and nutrition impacts only
Data summary
Biochemistry
Recent relevant available biochemistry indicates –
– marginal vit D – current intervention provides 50,000 IU/month. Recently checked and indicates now within acceptable range. Given Mr ACW’s range of diagnoses, including several that fall within the dysfunctional mitochondria umbrella, advisable to continue with current intervention.
Glycaemia
– before breakfast – 7.4-10.9; recommended range 4-6
– daily range – 7.4-19.8; recommended range 4-10
– reportable limits: < 3 and > 28
– checked weekly
– advisable to check HbA1c and clarify overall glycaemic control
Diabetes drugs
– glargine has a time to onset of 1 hour, minimal peak, and duration of 20-26 hours;
– metformin has a duration of 12 hours.
Diabetes drugs coverage
– before breakfast BSLs – minimal, if any, coverage from previous evening’s metformin; covered by previous evening’s glargine
– before evening meal BSLs – covered by current morning’s metformin, some coverage from previous evening’s glargine
Pharmaconutrition
Currently prescribed 3 medications that include nausea, vomiting and diarrhoea as side effects.
Cholecalciferol 50,000 IU/month provides the equivalent of 1,700 IU/day.
Coffee inhibits vitamin D uptake by osteoblasts (bone builders) by inhibiting their vitamin D receptors, and consequently decreases calcium and zinc absorption.
Metformin decreases Mg, B1, B6, B9, vit D, and B12 absorption – there is now a recommendation for B12 status to be monitored on a regular basis ie at least annually.
Dietary levels of caffeine intake in conjunction with paracetamol inhibit antinocieception.
Concurrent ingestion of paracetamol and iron resulted in increased rate of iron absorption and decreased extent of drug absorption; advisable for drug and iron to be administered at different times from each other.
Prolia increases risk of hypocalcaemia as it blocks calcium release from the bone.
Prolia associated with slight improvement in zinc and iron status and a decrease in copper, magnesium and phosphate levels; regular monitoring phosphate levels and concurrent magnesium intervention recommended.
Several of the identified membrane transporters inhibit the absorption and/or organ and cellular uptake of thiamine, choline, carnitine, pyridoxine, pantothenate, biotin and folate. Consequently, blood test results may be unreliable due to drug prevention of their entry into or exit from relevant organs and cells. Advisable for blood tests to be conducted several hours after administration of relevant prescribed medicines.
Bowel management
No regular intervention prescribed.
PRN aperient prescribed; administered 3 x Apr.
No Nurse Initiated interventions administered.
Staff comments
Staff advise Mr ACW has episodes of inexplicable vomiting and that he is recovering from a recent bout of influenza A.
Observations
Mr ACW was sitting in his room and was not his usual feisty self – likely due to recovering from influenza.
Mr ACW was weight stable until a recent hospitalisation so there is a likely subsequent weight loss.
Pharmaconutrition comments
Mr ACW’s diagnoses include deafness – nutritional factors to ensure within acceptable ranges include –
– B12 and/or folate – currently prescribed metformin therefore advisable to check B12 status and if low then intervention recommended;
– vitamin D – associated with low-frequency and speech-frequency hearing loss; currently prescribed metformin therefore advisable to clarify status.;
– thiamine – associated with bilateral hearing loss and proposed mechanism of action is that thiamine transporter OCT2 is expressed in the hair cells of the cochlea therefore interruptions to thiamine accessibility are likely to impact hair cell function; currently prescribed metformin which decrease thiamine availability both directly and indirectly.
Mr ACW’s diagnoses include chronic pain – nutritional factors that may be useful to consider in pain management include –
– vitamin D – evidence indicates increasingly brittle pain control with decreasing/low vitamin D levels. Advisable to monitor vitamin D levels on a regular basis and ensure they are not diminishing;
– low B12 exacerbates elevated TNF- α which is an inflammatory response marker; elevation of the inflammatory response can include a pain response and currently prescribed metformin therefore advisable to check B12 status;
– magnesium – proposed mechanism magnesium blocks the NMDA receptor channels in the spinal cord and thus limits the influx of calcium ie reduces the risk of excitotoxicity and consequent exacerbation of pain. Currently prescribed metformin which decreases magnesium absorption.
Mr ACW’s diagnoses include falls – nutritional factors that may be useful to ensure within acceptable ranges include –
– vitamin D – increasing vitamin D intake increases muscle strength and decreases falls; currently prescribed metformin and colecalciferol therefore advisable to clarify vitamin D status on an ongoing basis;
– B12 – is important in the righting reflex when a person stumbles; prescribed metformin therefore advisable to monitor status;
– iron – currently prescribed paracetamol therefore advisable to monitor status, and to check administration times in relation to each other;
– magnesium – magnesium is important in vitamin D activation, de novo carnitine production, and muscle function, amongst other functions. Also currently prescribed metformin which significantly decreases magnesium absorption. Magnesium is an intracellular ion therefore serum levels are unlikely to detect early depletion of status Advisable to monitor magnesium status.
What else would you include?

Yvonne Coleman is an accomplished dietitian with 30+ years of experience in aged care. Her mission is to make information concerning the interactions between medication and nutrition public and easy to access, having created the most comprehensive resource on the matter.
Her areas of competency include food science & nutrition, dietetics and health education. You can find out more about her work on LinkedIn, AusMed, the Enlightened Pharmacist podcast, and The FX Medicine Podcast.


