An aspirin-folic acid interaction was a recent “incidental finding” from a pooled analysis of some studies looking at brain atrophy response to a B vitamin intervention. The population-based studies consistently identified a negative aspirin-folic acid interaction in those with cognitive impairment, however the mechanism(s) of action remains speculative.
The aspirin-folic acid interaction was initially discovered in the 1970’s, and subsequently referred to in many texts published in the 1980s, 1990s, and 2000s. Clinical management strategies were never developed and so the interaction was “forgotten”. The attitude/belief that “old” research is not valuable is also a likely contributor to its “forgotten” status.
Proposed mechanisms of action include –
- Regulation of DHFR response. Folic acid is a synthetic form of folate that is ultimately converted to tetrahydrofolate by dihydrofolate reductase (DHFR). By inhibiting protein “E2F-1”, aspirin can regulate DHFR expression. Inhibition of DHFR upregulation can cause increased serum levels of unmetabolized folic acid. There is concern that unmetabolized folic acid may impair the transport of active folates into the brain.
- Inhibition of RFC-1. The reduced folate carrier-1 (RFC-1) transports reduced folate into the brain, and its inhibition will likely result in cerebral folate deficiency. The aspirin hydrolysate salicylic acid is a likely low-affinity inhibitor of RFC-1.
The evidence across the decades consistently indicates that aspirin consumers are at risk of impaired folate status, and that folic acid interventions are ineffective.
Clinical Considerations
If a folic acid intervention is to be considered when aspirin is prescribed then when would be the best time to administer it?
Given the recommended timing for aspirin administration is with food, perhaps folic acid interventions should be administered one hour prior to the same meal, to minimise exposure to any inhibitory effect.
Clinical Questions
What actions will you initiate as you a review a person whose prescribed medications include aspirin, will you –
- recommend regular monitoring of folate status?
- consider recommending a folic acid intervention, and at what time?
- if a folic acid intervention is prescribed and folate levels are high or at the high end of the acceptable range, will you question inhibition and therefore review administration time of the intervention in relation to aspirin administration?
- recommend the Medications Advisory Committee develop guidelines for folic acid administration when aspirin is prescribed?
Conclusions
The aspirin-folic acid interaction has been recently rediscovered. Perhaps this time clinical management strategies will be developed and introduced to ensure its long-term negative impacts do not continue.
Medical History with Nutritional Aspect
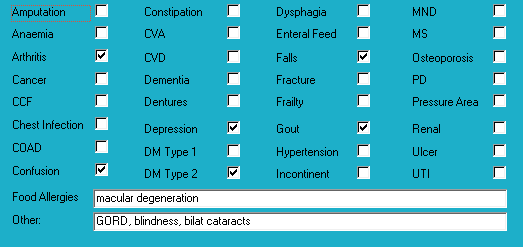
Biochemistry with Nutritional Aspect
No recent relevant results available.
Medications That May Adversely Affect Nutritional Status
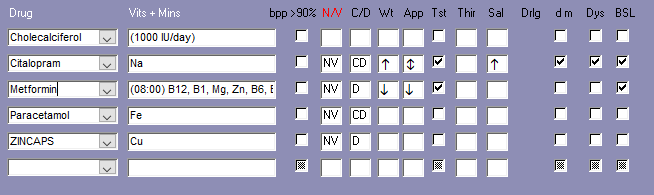
Transporter-mediated interactions and nutrients
Comments – medication and nutrition impacts (direct and indirect) only
Data summary
Biochemistry
No recent relevant biochemistry available.
Glycaemia
BSLs (Aug-Oct) –
Before breakfast – 6.3-8.1; recommended range 4-6
Tested weekly.
Reportable limits: < 4 and > 20.
HbA1c indicates very good overall glycaemic control.
Diabetes drugs
– metformin has a duration of 12 hours
Diabetes drugs coverage
– before breakfast BSLs – no coverage from previous morning’s metformin;
– before evening meal BSLs – covered by current morning’s metformin.
Currently prescribed 3 medications that alter glycaemia.
Pharmaconutrition
Currently prescribed 4 medications that include nausea, vomiting and diarrhoea as side effects.
Currently prescribed 3 medications that include anaemia as a side effect.
Coffee inhibits colecalciferol uptake by osteoblasts (bone builders) by inhibiting their vitamin D receptors, and consequently decreases calcium and zinc absorption therefore regular monitoring zinc status recommended.
Both citalopram and paracetamol are CYP1A2 inhibitors (blocks transporter function). CYP1A2 substrates include caffeine, retinol, melatonin, phosphatidylcholine, inhibitors include grapefruit juice and inducers include coffee; drug’s metabolism inhibited therefore the drugs will remain active in the body for longer.
Regular monitoring sodium levels recommended whilst citalopram prescribed.
Metformin decreases Mg, Zn, B1, B6, folate, and B12 absorption – there is now a recommendation that B12 levels be checked on a regular basis ie at least annually; advisable to also monitor Mg, Zn, B1, B6, folate on a regular basis ie at least annually.
Dietary levels of caffeine intake in conjunction with paracetamol inhibit antinocieception.
Concurrent ingestion of paracetamol and iron resulted in increased rate of iron absorption and decreased extent of drug absorption; the authors advise drug and iron to be administered at different times from each other.
Longterm zinc administration may cause copper deficiency as they share the same absorption mechanism.
Zinc caps have been prescribed for 8 months, and sozole intervention has been ceased therefore advisable to check zinc levels and if > 11 units then review necessity for its continued prescription.
Currently prescribed vitamin D (1 tab/day). Advisable to check vitamin D levels and if still low then review current vitamin D management strategy.
The identified membrane transporters inhibit the absorption and/or organ and cellular uptake of thiamine, choline, carnitine, NMN (B3), pyridoxine, folate, and pantothenate which means blood test results are likely to indicate normal or elevated status whereas these nutrients may be in the blood because they are prevented from entering relevant organs and cells. Advisable for blood tests to be conducted several hours after administration of relevant prescribed medicines.
Bowel management
Regular intervention prescribed – no.
PRN interventions prescribed – no.
Nurse Initiated interventions administered – no.
Staff comments
Staff advise Mrs ACQ eats well and does not have significant food restrictions.
Observations
Mrs ACQ is a small lady with a large abdo and who was lying on her bed when I went to speak to her – she told me she eats well, sleeps well, does not feel upset in the tummy, and sometimes goes outside if the sun is shining.
Mrs ACQ has remained remarkably weight stable about 58 kg for the last 3.5 years.
Pharmaconutrition comments
Metformin is administered in the mornings therefore advisable to check afternoon/before-evening meal glycaemia for 3 days and clarify status. Staff advise Mrs ACQ does occasionally graze in the afternoons. Mrs ACQ’s diabetes management includes 1 drug administered before breakfast and which has a duration of about 12 hours. If the 3 days of afternoon glycaemia monitoring indicate hyperglycaemia then it could mean
- current medication management strategy is undermedicating glycaemic control and therefore requires review;
- current medication management strategy is overmedicating glycaemic control and causing the liver to release stored glucose as a hypoglycaemia management strategy and therefore medication strategy requires review;
- current medication management strategy is overmedicating glycaemic control and Mrs ACQ is grazing to offset the hypoglycaemic effect and therefore medication strategy requires review;
- current medication management strategy is overmedicating glycaemic control and causing both the liver to release stored glucose and Mrs ACQ to graze and therefore medication strategy requires review.
Mrs ACQ’s diagnoses include arthritis which means chronic pain – nutritional factors that may be useful to consider in pain management include –
– vitamin D – current intervention may not be adequate to attain adequate range. Evidence indicates increasingly brittle pain control with decreasing vitamin D levels. Advisable to check vitamin D levels and if still low then review current vitamin D management strategy
– low B12 exacerbates elevated TNF- α which is an inflammatory response marker; elevation of the inflammatory response can include a pain response and currently prescribed metformin therefore advisable to check B12 status. There is disagreement between pathology ranges and research findings with regard to appropriate B12 levels – neuro-imaging evidence indicates B12 interventions are effective once levels are less than 300 pmol/L;
– magnesium – proposed mechanism magnesium blocks the NMDA receptor channels in the spinal cord and thus limits the influx of calcium ie reduces the risk of excitotoxicity and consequent exacerbation of pain. Currently prescribed metformin which decreases magnesium availability.
Mrs ACQ’s diagnoses include falls – nutritional factors that may be useful to consider in falls management include –
– low B12 – is important in the righting reflex when a person stumbles; prescribed metformin therefore advisable to check status;
– low magnesium – magnesium is important in vitamin D activation and muscle function, amongst other functions. Also currently prescribed metformin which significantly decreases magnesium availability. Magnesium is an intracellular ion therefore serum levels are unlikely to detect early depletion of status Advisable to clarify magnesium status.
Mrs ACQ’s diagnoses include diabetes and gout – and both are now linked to dysfunctional mitochondrial. Some key nutrients in mitochondrial function include –
– magnesium citrate – important in the electron transport chain (etc) and oxidative phosphorylation;
– thiamine – deficiency impairs oxidative phosphorylation.
Both of these nutrients are negatively impacted by metformin prescription.
What else would you include?

Yvonne Coleman is an accomplished dietitian with 30+ years of experience in aged care. Her mission is to make information concerning the interactions between medication and nutrition public and easy to access, having created the most comprehensive resource on the matter.
Her areas of competency include food science & nutrition, dietetics and health education. You can find out more about her work on LinkedIn, AusMed, the Enlightened Pharmacist podcast, and The FX Medicine Podcast.


